Trends in Social Innovation: Health and Vitality
According to the World Health Organization, the United States spends more per capita on health care than any other nation in the world. But despite America’s heavy spending, the 2000 World Health Report ranked it a dismal 37th in a line-up of 191 countries in quality of health care. In 2012, according to the CIA World Factbook, the infant mortality rate—a key indicator of a country’s health—was 6 deaths per 1,000 live births in the United States. Comparatively, nations such as France, Italy, and Singapore which spend less or considerably less on health care than the US all had lower infant mortality rates.
It’s apparent from this data that America has an embarrassing efficacy problem when it comes to health care. Every year, Americans spend increasing amounts for health insurance and medical services, but it is disputable whether we are becoming a healthier nation as a result. The current public debate over health care fails to give sufficient attention to the fact that real health is not something that can be purchased through a transaction or received from the government, but is rather a state of being that must be cultivated through a culture that understands and respects the human traditions of healing. Real health should be defined not as “lack of disease” but rather as a vitality which encompasses not simply the physical, but also the mental, spiritual, social, economic and environmental aspects of human life.[1]
What we have labeled as “health care” is really just “medical intervention”—a fee-for-service model in which consumers pay health providers for itemized services (doctor’s visits, tests, vaccinations, surgeries, etc.). Medical intervention, however, is only a small slice of what it takes to foster health and vitality. In fact, medical intervention should only be an emergency response to the physical break-down of the human body, and health care should be those things we do to keep a person in full wellness.
Because we have reduced our understanding of health to this very narrow—albeit important—element called medical care, we have allowed ourselves to fall prey to divisive policy debates about who is going to pay for and regulate medical insurance, too often neglecting our own natural ability and responsibility as individuals and communities to foster holistic, vital lives.
Heather Wood Ion, founder of The Epidemic of Health and senior fellow of The Philanthropic Enterprise, points out that “the vector of health is a vital person.” Coming at health from this angle, is it possible to harness this vitality and move America toward a healthier future?
Grasping a few key principles will help get us there:
Individuals have the capacity to pursue their own vitality.
The current medical culture tends to treat individuals as passive recipients of medical goods and services. Subsequently, people begin to believe that they are simply helpless patients, instead of proactive consumers who can decide what’s best for their own health. Approaches that empower individuals to cultivate their own health and to participate in decisions about medical services when they are needed reinforce the truth that people are moral agents who can take responsibility for their own well being. In this series, we will examine several groups that are doing just that—educating and encouraging people to sit in the driver’s seat of their health future.
Healing is anchored in the community.
In the recent past, we have adopted an overly individualized approach to health, ultimately creating a disconnectedness, an isolation which contributes to the notion that one is alone—except for the role of the medical provider—in the healing journey. This view completely ignores the role of the larger community in contributing to and supporting the individual’s healing and vitality—a perspective that was historically the norm.
“In our discussions of crises in medical care and medical policy, we too often forget that healing takes place outside medical systems and institutions: while an intervention may begin a recovery process, it is in the interactions of our lives that we heal, care and restore our vitality,” says Ion.
Vitality springs from prevention, not remediation.
Wellness and wholeness flourish when people approach their health through eyes of prevention. Remediation, or medical intervention, should be a last resort, not a first step. For instance, eating healthfully and exercising regularly should be viewed as the foremost “cure” for obesity, not diet pills or gastric bypass surgery after obesity has already set in.
True vitality embraces life’s natural courses.
Austrian philosopher Ivan Illich in his book Medical Nemesis: The Expropriation of Health refers to the “medicalization of life” in modern American culture. What he’s talking about is the odd and unnecessary “medicalizing” of issues which people were historically capable of dealing with without medical intervention. Some view the labeling and medicating of the childhood “malady” of ADHD as an example of applying a superfluous solution to a condition that is often attributable to external, not physical, factors. A shocking example in a recent New York Times article describes how doctors are doling out ADHD medication to help children who are performing poorly in school, supposedly because some parents and schools would rather medicate than deal with the real issues behind a child’s poor performance.
Throughout history, individuals—through the support of their families, neighborhoods, religious communities, and other organic networks—have been dealing with life’s ups and downs, including death, with a gracious understanding that there is a “time for everything.”[2] Our modern approach to “health care” has tended to relegate this way of thinking to the sidelines, but groups of citizens across the country are finding creative ways to bring individuals back to the center of their health decisions, incorporate community support in the healing process, promote a preventative way of life, and celebrate human resilience in the natural course of life.
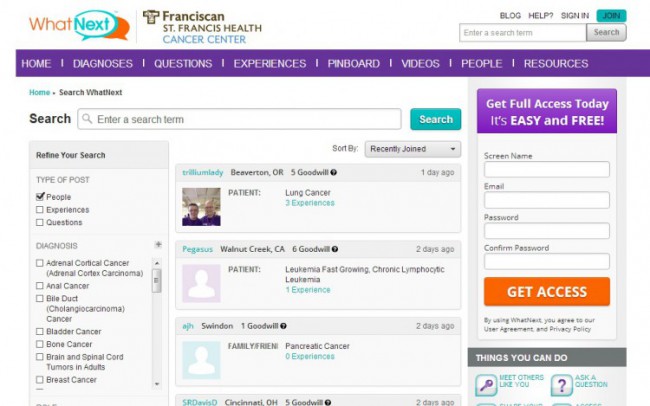
In this series in Trends in Social Innovation, we will begin by looking at three approaches to boosting human health and vitality. In “Lunch Break Health Care” we explore a groundbreaking approach to employer-based health care that prioritizes disease prevention as a way to save money. In “Free to Share” we take a look at a network of individuals who pay for each other’s medical expenses, bypassing insurance systems completely. And in “Algorithmic Remedies” we introduce two online tools that enable individuals to look to fellow patients for help navigating the complexities of medical services.